What is the Multi-County eConsult Initiative?
MCEI is a partnership between Inland Empire Health Plan (IEHP), Arrowhead Regional Medical Center (ARMC) and Riverside University Health System (RUHS) to improve access to care for the Safety-Net population through practice transformation in San Bernardino and Riverside counties. IEHP is sponsoring the initiative to design, implement and evaluate eConsult at more than 150 clinic sites with the ultimate goal of 100% participation from providers throughout both counties.
- Mission: Increase access to specialty care
- Vision: Provide eConsult to safety-net patients, for all primary care providers, and across all specialties.
- Objectives:
- Improve access to health care
- Increase access to timely specialty care for members
- Improve communication
- Allow PCPs and specialists to hold a digital dialog and co-manage a patient’s case
- Expand primary care practice scope via case-based learning
- Improve efficiency
- Ensure appropriate visits, resolve unnecessary visits
- Improve pre-visit workup
- Improve access to health care
What is eConsult?
Short for “electronic consultation,” eConsult is a virtual care coordination process that enables Primary Care Providers (PCPs) to message Specialists regarding patient care and the need for specialty referral. PCPs may pose a simple question (e.g., about a drug dosage) or a more complex question following an initial assessment (e.g. asking for a virtual dermatology assessment and providing images of the patient). A secure web-based application facilitates this message exchange, allowing specialists to respond, usually within a day, to PCPs’ questions.
Through this PCP-Specialist dialog, all patients gain virtual access to specialty care and can obtain referrals in a quicker, more efficient manner. These virtual interactions are crucial to the success of reducing patient visit wait times, unnecessary appointments, and appointment no-shows.
The Problem? A Broken Referral Process
Forty percent (40%) of referrals lack one or more of the three key elements for a successful referral: medical necessity, correct specialty, and complete workup (Chen et al.). In the traditional referral process, relevant information and background is often lost, thus delaying care plans and creating duplicate tests and procedures. Such motions are costly and time consuming for all parties involved, and creates potentially harmful delays for patients in particular. There is ample evidence to suggest that failures in care coordination via the referral process negatively impact patient care (Horner et al., OMalley et al.)
Analysis revealed a 20-step referral process, with 8 different people and record systems involved; more steps means more potential “break points,” where one error can “dramatically decrease the chance that the patient would ever see the specialist” and get the care they need. An average of 2 of every 5 referrals get scheduled, and of those patient who do get an appointment, 40% do not show up. The issues of inefficient referrals, scheduling failures, and the no-show rates combined impact Medicaid patients in a particular way, since they are usually in poor health with higher rates of disability, fewer economic resources, limited mobility, and more to lose when missing work for care.
The Solution? Practice transformation through eConsult.
Overall documented impact includes:
- Access: Patients arrive at specialty appointments with the appropriate work-up and shorter wait times.
- Connect: eConsult reduces unnecessary referrals to specialists and focuses treatment for patients on a priority basis. Specialists receive clear clinical questions, and related documentation that provides more-efficient referrals.
- Inform: eConsult is a platform for specialists to exchange educational material with referring clinicians, providing "just-in-time" education, which is applied right away. This allows the requesting clinician to remain the main contact for their patients. Primary care physicians receive timely input and expertise from specialists
- Value: Reduces no show rates by increasing productivity of an appointment interaction by ensuring diagnostic workups are complete. Primary care physicians and specialists utilize an interdisciplinary approach though establishment of common expectations before and after a referral has been made. The quality of care provided at the Institutional level improves.
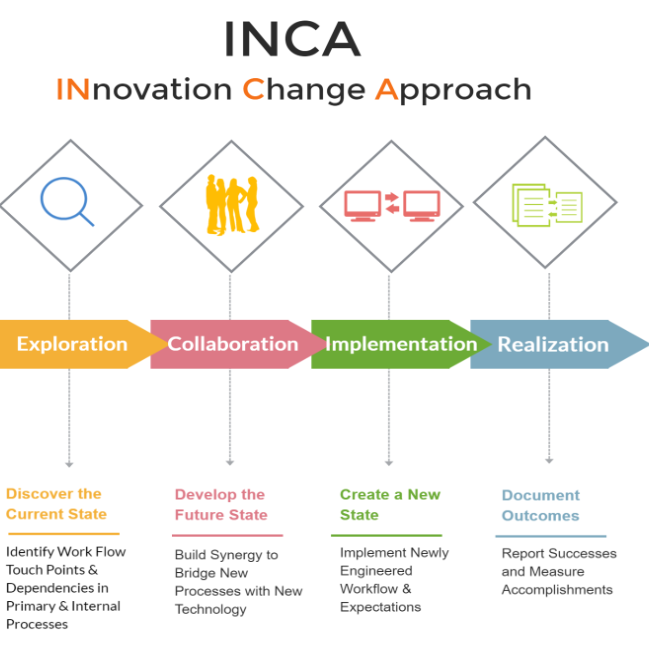
Innovation Change Approach or INCA is a refined method that draws from Design Thinking, LEAN Six Sigma, Human-Centered design, Agile Method, and Continuous Process Improvement. INCA focuses on behavior and workflow processes by looking at potential efficiencies and improvements as part of a four-step approach to practice transformation.
1) Exploration, understand the current state
2) Collaboration, collectively develop -future state
3) Implementation and application of improved
4) Realization, conclude with thorough and ongoing realization.
Benefits include: thorough assessments with clear process mappings, better team buy-in to the project, and reduced time to full and effective implementation. This approach helps reduce costs and time to complete a project by effectively reducing the time at the front end, the current state evaluation and future state development, and still providing deep analysis and rapid and creative ideation. Most importantly, INCA is a highly effective and proven way that Wise can execute practice transformation.

